Three Unique NICU Journeys
Delivered via C-section shortly after Maria arrived at CHRISTUS Children’s, all three babies were rushed to the NICU. Brayden and Audrina were small and initially healthy, but both would soon require specialized care.
Brayden was breathing well, so we removed his breathing tube, to allow him to breathe on his own and help his lungs grow stronger,
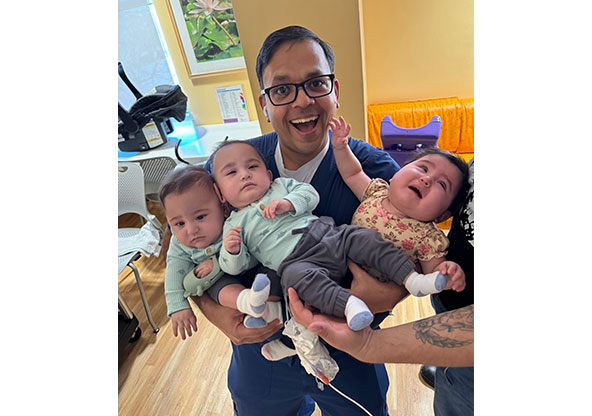
explained Dr. Pratik Parikh, neonatologist and assistant medical director of the CHRISTUS Children’s NICU. In premature babies, even small changes can overstimulate their fragile systems and lead to complications, and that’s what happened with Brayden.
Brayden began to have trouble breathing, putting stress on his lungs and brain. He was quickly treated with a specialized procedure and soon began to grow stronger. It was also discovered that part of his bowels had not fully formed, and Dr. Chris Westgarth-Taylor, director of the Pediatric Colorectal and Urogenital Program, performed surgery to remove the unhealthy tissue, allowing for normal digestion.
On October 23, Brayden was well enough to go home, the first of the triplets to reach that milestone. Meanwhile, his sister Audrina had been doing well until she suddenly stopped eating.
Like many premature babies, she tired easily and would forget to eat or wouldn’t eat long enough to get the nutrients she needed,
Dr. Parikh said. We placed a gastrostomy tube, or G-tube, into her stomach to ensure she received adequate nutrition.
Audrina was also the first of the triplets Maria was able to hold.
She was about five days old, and she was so little,
Maria recalled. was able to do skin-to-skin with her, and I cried because I was so happy. That was a very special and emotional day.
Audrina was discharged home on November 18, and she continues to receive speech therapy to help improve her feeding and swallowing skills. Over the next three months, Maria, Brandon, Brayden and Audrina would make regular trips to visit Cody.
Beating the Odds: Cody’s CDH Surgery
At birth, Cody was too fragile to undergo the surgery needed to repair his diaphragm,
explained Dr. Parikh. All of the odds were against him, so I spent many late nights monitoring Cody and working to stabilize his breathing and oxygen levels.
When Cody was about one month old, Dr. Parikh believed he was finally strong enough for surgery—an extraordinary milestone as Dr. Parikh had never seen a baby this premature undergo CDH repair surgery at such a young age.
The entire NICU team never shied away from hard conversations, Maria said. We appreciated that they wanted us to be prepared, and they were always so compassionate. I remember when Dr. Parikh told us he thought Cody was ready. We knew there were risks involved with surgery, but we also knew Cody wouldn’t survive without it.
On July 23, Dr. Jonathan Greenfeld, a pediatric surgeon, operated on Cody, moving his abdominal organs into their proper place and surgically repairing his CDH.
At just 950 grams (2 pounds, 2 ounces), Cody was less than half the size of most babies who undergo this type of procedure. Making things even more complex, he was missing his entire left diaphragm—a rare and serious form of CDH. The condition already carries a 50% mortality rate in full-term babies, and while there’s no specific data for extremely premature infants like Cody, experts estimate the risk could be as high as 75 to 90%.
Against all odds, Cody has had no major complications and has not needed another surgery—something that happens in about 25% of CDH cases, even in full-term babies.
This was an extremely complex and technically challenging procedure,
said Dr. Greenfeld. I was so glad to see him come through it so well. It was truly an honor to care for such a wonderful family, and I’m incredibly happy to see Cody growing, thriving and beating the odds.
Cody’s outcome, against all odds, was a significant milestone for the care team.
The surgical team did an outstanding job treating Cody,
Dr. Acosta said. While CDH is still a serious diagnosis, Cody’s story should give parents hope. With early intervention and the right care team, we were able to give the smallest, most fragile Hernandez baby a fighting chance.
A few weeks after Cody’s successful surgery, Maria shared with one of the NICU nurses that Cody was the only baby she hadn’t been able to hold yet due to concerns about his fragility.
We met so many incredible nurses throughout our journey, and there was something extra special about Kristen,
Maria said. When she found out I hadn’t held Cody yet, she gave me her work schedule and told me to come in when she was on duty. On my next visit, I got to hold him. Kristen took pictures and even did a video call with Brandon so he could be part of the moment. When she was assigned to Audrina, Kristen would dress her up in a cute outfit and send us pictures. She was just there for me in such a special way.
Thriving at Home Together

Finally, on February 28, more than eight months after the triplets were born, Cody was discharged, and the siblings recently celebrated their first birthday.
I never thought this would be my life, but I love it so much,
Maria said. We have our routine, and the babies are doing great. My miracle babies are the best thing that ever happened to me. I’m so thankful for the CHRISTUS Children’s team because they cared for us every step of the way, and they continue to help Cody, Brayden and Audrina thrive.
That’s what we’re here for,
said Dr. Parikh. Our NICU team is renowned for the family-centered care we provide. We don’t just take care of the babies, we support the entire family in their NICU journey from birth to discharge.
At CHRISTUS Children’s, every baby and family receives expert, compassionate care, no matter how complex their journey. Learn more about the Level IV NICU at CHRISTUS Children’s, visit CHRISTUS Children's.